Learn About Blood Clots
Understanding Blood Clots: An Essential Overview
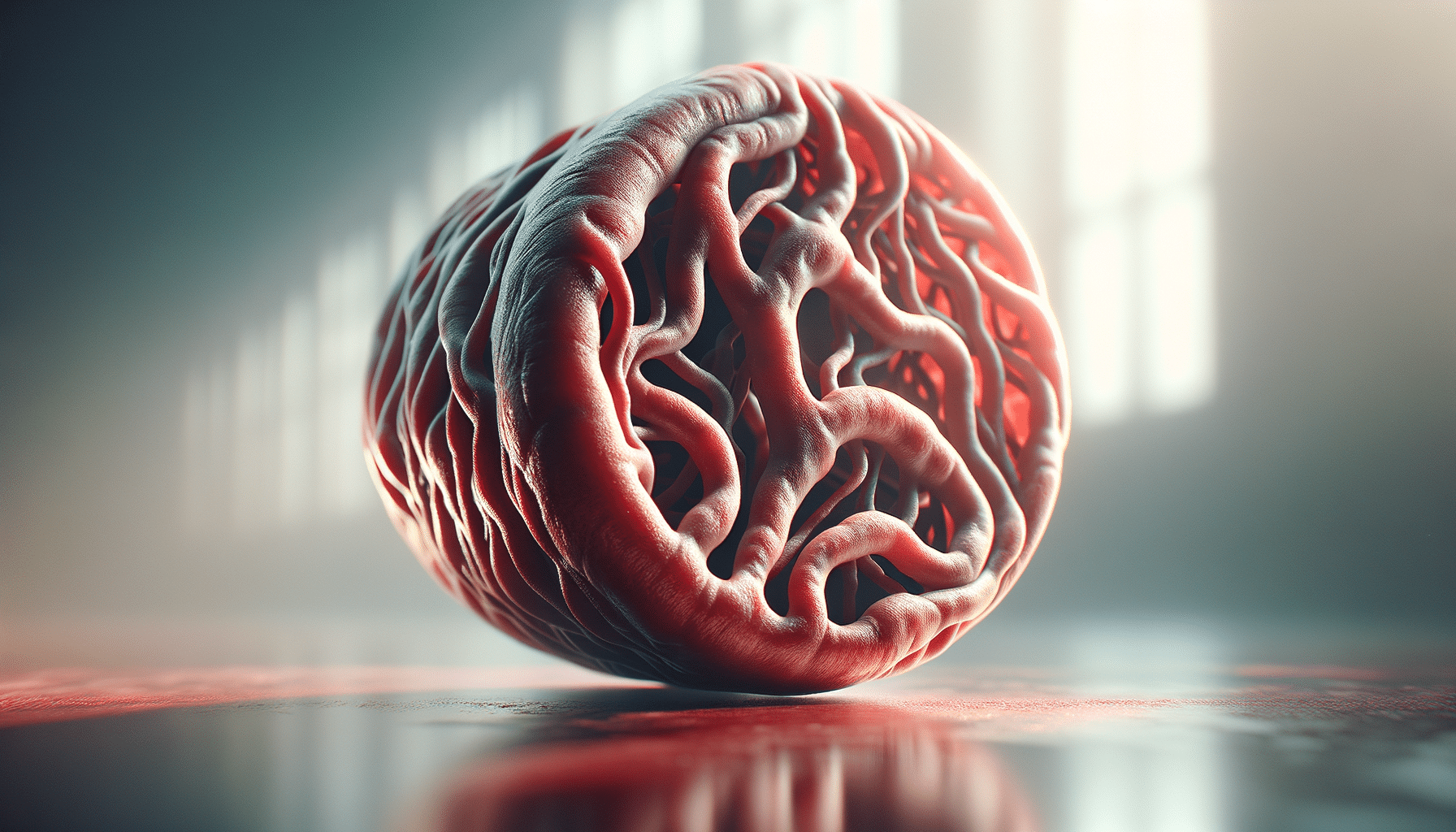
Blood clots are a crucial aspect of the body’s natural healing process, but they can also pose significant health risks if not properly managed. Understanding what blood clots are and how they function is vital to maintaining overall health. Clots form as a response to injury, preventing excessive bleeding by solidifying blood at the site of a wound. This process, known as coagulation, involves platelets and proteins working in tandem to form a stable clot.
However, not all blood clots are beneficial. When clots form inappropriately within blood vessels, they can obstruct blood flow and lead to serious medical conditions such as deep vein thrombosis (DVT) or pulmonary embolism. These conditions can result in severe complications, including stroke and heart attack, highlighting the importance of recognizing the symptoms and risk factors associated with blood clots.
Common signs of blood clots include swelling, pain, tenderness, and redness in the affected area. Identifying these symptoms early can significantly improve treatment outcomes and reduce the risk of complications. Being informed about blood clots empowers individuals to seek timely medical intervention, ultimately safeguarding their health.
The Mechanism Behind Blood Clot Formation
The process of blood clot formation is a complex yet fascinating mechanism involving various components of the blood. When a blood vessel is injured, the body initiates a series of events collectively known as the coagulation cascade. This cascade involves the activation of clotting factors, which are proteins essential to the clotting process.
Platelets, small cell fragments in the blood, play a pivotal role in clot formation. Upon injury, they rush to the site and adhere to the damaged vessel wall, forming a temporary plug. This action triggers the release of chemical signals that activate clotting factors, leading to the conversion of fibrinogen, a soluble protein, into fibrin strands. These strands form a mesh that solidifies the platelet plug, creating a stable clot.
While this process is vital for healing, it must be tightly regulated. An imbalance in clotting factors or platelet function can result in excessive clotting or bleeding disorders. Conditions such as hemophilia, where clotting factors are deficient, exemplify the need for precise control within the coagulation system. Understanding this delicate balance is crucial for developing effective treatments and preventing clot-related complications.
Risk Factors Associated with Blood Clots
Several factors can increase the likelihood of developing blood clots, making it essential to recognize and manage these risks. Lifestyle choices, medical conditions, and genetic predispositions all play a role in clot formation. Being aware of these factors can help individuals take proactive measures to reduce their risk.
Some common risk factors include prolonged immobility, such as during long flights or bed rest, which can lead to conditions like deep vein thrombosis. Additionally, certain medical conditions, including obesity, cancer, and heart disease, are associated with an increased risk of clotting. Pregnancy and hormone replacement therapy can also elevate the risk, particularly in women.
Genetic factors, such as inherited clotting disorders, can predispose individuals to excessive clot formation. Family history of blood clots can be a significant indicator, necessitating regular check-ups and possibly genetic testing. By understanding and managing these risk factors, individuals can take steps to prevent blood clots and maintain cardiovascular health.
Diagnosis and Treatment of Blood Clots
Accurate diagnosis of blood clots is crucial for effective treatment and prevention of complications. Healthcare professionals employ various diagnostic tools to identify clots and assess their severity. Common diagnostic methods include ultrasound imaging, which visualizes blood flow and detects abnormalities, and blood tests that measure clotting factors and markers of clot formation.
Once diagnosed, treatment strategies aim to dissolve the clot and prevent further clotting. Anticoagulant medications, commonly known as blood thinners, are often prescribed to reduce the risk of clot formation. These medications work by inhibiting specific clotting factors, thus preventing the coagulation cascade from progressing.
In some cases, more aggressive treatments may be necessary, such as thrombolytic therapy, which involves administering drugs to dissolve the clot directly. Surgical intervention might be required to remove large clots or those that pose an immediate threat to vital organs. Early diagnosis and treatment are key to preventing severe complications and ensuring positive health outcomes.
Preventive Measures and Lifestyle Modifications
Prevention of blood clots involves a combination of lifestyle modifications and medical interventions tailored to individual risk factors. Engaging in regular physical activity is one of the most effective ways to reduce the risk of clot formation. Exercise promotes healthy blood circulation, preventing the stagnation that can lead to clotting.
Maintaining a balanced diet rich in fruits, vegetables, and whole grains supports overall cardiovascular health. Limiting the intake of saturated fats and cholesterol can also reduce the risk of conditions that contribute to clot formation. For individuals at high risk, healthcare providers may recommend regular monitoring and possibly prophylactic anticoagulant therapy.
Additionally, avoiding smoking and excessive alcohol consumption is crucial, as these habits can adversely affect blood vessel health and increase clotting risk. By adopting a healthy lifestyle and working closely with healthcare professionals, individuals can significantly lower their chances of developing blood clots and enjoy a healthier life.